About this series:
At Revent, we invest in solutions tackling the biggest problems in planetary and societal health. The COVID-19 pandemic shed light on deep vulnerabilities within our healthcare systems, spurring our team, like many others, to do some serious thinking about why and what can be done.
In our inaugural Revent Reflections series, we present our thesis on one part of the puzzle: preventive health, its enormous impact potential, and the myriad of opportunities to build within it.
This will be a multi-part series researched and released over the next few months. This introductory piece serves as an overview of Preventive Health and what we’ve identified as unifying problems within the space. In upcoming pieces, we will dig deeper into these challenges and consider how they can be solved.
Summary
🤷♀️ What’s the problem?
Consider these two statistics:
An estimated 80% of cases of cardiovascular disease, the leading cause of death in Europe, are preventable.
The average EU country spends just 3% of its annual healthcare budget on preventive care, compared to 53% on curative and rehabilitative care.
As our population ages, we are increasingly burdened by chronic conditions that develop over the course of decades, stemming from an evolving and interwoven set of genetic, behavioral, and environmental factors.
Preventive medicine has emerged as a promising antidote, but our health systems have not caught up.
🤕 What’s preventing the prevention?
We’ve identified three overarching challenges that must be addressed for prevention to become a dominant force within our healthcare systems. See the full article below for details, but here are the high-level takeaways:
Lack of motivation: “Preventive health is like eating spinach - you know it’s good for you but you still don’t do it.” Stronger incentives are needed for healthy individuals to take preventive measures and for those with chronic diseases to adhere to management regimens.
Unaligned system-wide incentives: The economic incentives of preventive health lie with organizational stakeholders (payers and employers), but behavioral change remains an individual’s responsibility.
Lack of (actionable) information: From fitness trackers to genetic screening, the field of available health metrics is growing in type, quantity, and complexity. This means the need is greater than ever for data to be more efficiently collected, processed, and synthesized into evidence-based recommendations.
👀 What does innovation in preventive health look like?
Did you know that there are four stages of preventive healthcare, ranging from improving lifestyle habits to avoiding medical harm? To learn more, check out the Opportunity Overview and Preventive Health Market Taxonomy.
🔍 What are we looking for?
Across the four stages of prevention, we are looking for startups targeting the most pressing causes of lifespan and healthspan loss and, while addressing at least one of the three challenges outlined above:
Primary prevention solutions help avoid altogether the onset of a disease, for example by integrating different data types (genetics, physical activity, sleep, blood biomarkers, microbiome, etc.) into evidence-based recommendations to drive behavioral change.
Secondary prevention solutions detect conditions early and treat them before they become severe, for example, through more accurate or accessible screening methods targeting commonly under- or mis- diagnosed conditions.
Tertiary prevention solutions help manage an existing disease to minimize its harm or burden on the patient, for example by lowering the cost & effort of monitoring, improving regimen adherence, and preventing the need for acute treatment.
Quartenary prevention solutions protect patients from medical harm, such as unnecessary or erroneous treatment, for example by empowering doctors to make better decisions in rare or complex cases.
We love to hear from founders, experts, and other investors in this space! Reach out at sharon@revent.vc.
Why prevention?
Key Trend #1: We are increasingly killed by chronic conditions, rather than acute or infectious ones.
Let’s go back to the year 1884, when German Chancellor, Otto von Bismarck, instituted the world’s first instance of compulsory health insurance. What did it mean to be sick back then? Well, the average German was expected to die before age 40. The most likely cause? Pneumonia or tuberculosis. This was representative of the reality worldwide, and that throughout most of human history - people died at relatively young ages from acute infections that spread from person to person.
What Bismarck could not have foreseen was that a century later, a medical revolution would redefine our understanding of illness. This diagram (source) shows how the top causes of death in England have evolved over the 20th century:
In many ways, this is a story of medical triumph. With the introduction of antibiotics and new vaccines in the early 1900s, infections ceased to be fatal. Economic development further extended life expectancy. By the 1960s, the majority of deaths were caused by cardiovascular disease and cancer. Today, these remain the leading causes of mortality across Europe, a trend that will likely continue as the population ages.
Similar transitions are now occurring globally in populations across Asia, Africa, and South America, spurring the WHO to make a formal case for global investment in chronic (aka non-communicable) diseases in 2021. In Europe, the organization set up an Advisory Council on Innovation for Noncommunicable Diseases in 2022.
Key Trend #2: We have been extending life but not ensuring health.
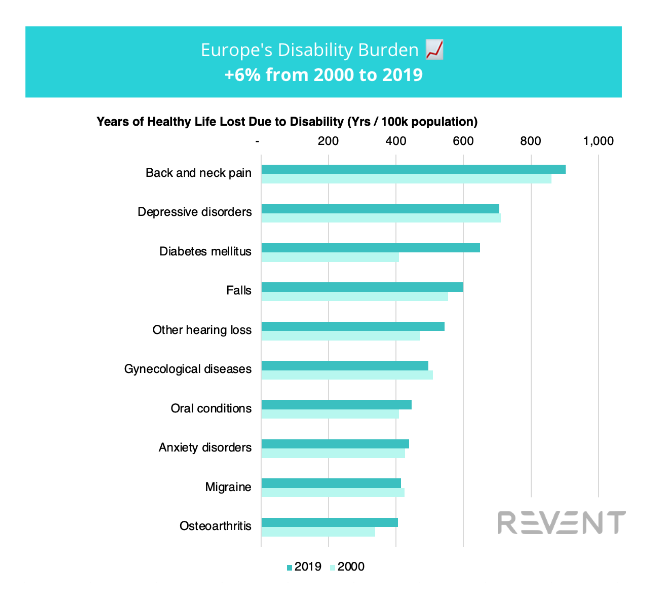
Take a look at the graph below. At first glance, we are finding success in our newfound battle with chronic conditions. From 2000 to 2019, European countries made progress on 9 out of the top 10 causes of premature mortality. Correspondingly, life expectancy has continued to increase.
Data Source: WHO
Yet, avoiding death is not all that matters. What does data tell us about our quality of life, not just length of life? Looking at the WHO’s measure of healthy lifespan (lower graph), a more complicated picture emerges. In contrast to the progress we’ve made on the top causes of death, we’ve been backsliding on the conditions that cause us to live less healthy lives. Note also the pronounced differences between the illnesses on these two lists - cardiovascular diseases and cancers kill, while chronic pain, mental health conditions, and diabetes cause people to suffer.
Data Source: WHO
Solving for mortality has not inherently improved quality of life. Instead, we are increasingly burdened by conditions that develop over the course of decades, partially stemming from a complex set of behavioral factors encompassing exercise, diet, and sleep. And, as demonstrated by the skewed impacts of the COVID-19 pandemic, these factors intersect deeply with socioeconomic status, education, and communal environments.
What’s the Problem, and Why Now?
These trends have posed an immense challenge to our healthcare systems. Germany’s Bismarckian health insurance was first implemented in 1884, while the UK’s National Health Service was established in 1948. These systems, initially designed to treat acute conditions, are struggling to adapt to the growing prevalence of chronic conditions, for which prevention matters as much as treatment.
To put this into perspective, in 2020, the average EU country spent just 3% of its healthcare budget on preventive care (mostly vaccinations and screenings for cancer and high blood pressure), compared to 53% on curative and rehabilitative care.
This challenge extends beyond the current scope of our healthcare systems. Potent levers for chronic diseases lie well before the point of diagnosis - consider the fact that an estimated 80% of Type 2 diabetes cases are preventable through lifestyle adjustments. Addressing the root cause for these conditions entails 360° involvement of individuals and their communities, from family members to employers, starting from birth. Yet, today, most of our intervention toolkit is only available after diagnosis, the gating point for attention and resources from most formal healthcare systems.
Fortunately, the landscape is beginning to shift. Evidence continues to accumulate that preventive medicine can help improve health outcomes and, in some cases, lower overall healthcare costs. Following the outbreak of the COVID-19 pandemic, the United States announced its aim to transition all Medicare (65+) beneficiaries to value-based care systems by 2030. In 2021, the EU began a 5.3 billion euro EU4Health Programme, including a particular focus on health promotion and disease prevention. Add to this technological developments from AI breakthroughs to digital diagnostics. The time is ripe to re-equip our healthcare systems to boost population-wide health with unprecedented precision, efficiency, and reach.
This is why we, at Revent, see a pressing need (read also: big opportunity) to shift our healthcare emphasis from reactive treatment to proactive prevention. The problem is clear. Our job now is to find and support those who are building the solutions.
Our Problem Thesis:
What’s preventing the prevention?
In this transition, there are a plethora of opportunities for visionary, fast-moving teams to move the needle. In particular, we are looking for startups building solutions that:
Target prevalent chronic conditions that cause not just loss of life, but loss of quality of life, such as chronic pain, depression, and diabetes (see Key Trend #2 above), and
Address cross-cutting barriers to prevention, including lack of motivation, unaligned system-wide incentives, and lack of actionable information (more details below)
To expand on this latter point, we’ve identified three unifying challenges for why the benefits of preventive health have been hard to realize. In our view, effective solutions must address some or all of these challenges:
Challenge 1: Lack of motivation
Stronger incentives are needed for healthy individuals to take preventive measures and for people with chronic diseases to better adhere to management regimens.
“Preventive health is like spinach” - even if we know certain behaviors support health, we might not do them because they require more effort or are less enjoyable.
Healthy individuals tend to be unmotivated to pay for their own preventive measures, especially before they become ill, requiring innovative approaches to build sustainable businesses in this space.
Patients with chronic diseases struggle to adhere to management measures - for instance, studies show that across European countries, around half of patients with hypertension fail to adhere to their treatment regimen.
To address this challenge, we are interested in scalable technology and business models that either increase motivation or reduce the need for it, such as:
Gamification, socialization, and accountability strategies with demonstrated effectiveness
Financial incentives
Prevention and disease management regimens that produce comparable outcomes while requiring less effort
Lack of motivation - case in point:
Noom and Weight Watchers, known for their focus on behavior change, have now started offering injectable medications for weight loss.
Challenge 2: Unaligned system-wide incentives
The economic incentives of preventive health lie with organizational stakeholders (payers and employers), but behavioral change remains an individual responsibility.
Aside from limited health screening, involvement in formal healthcare systems begins at the time of diagnosis, meaning earlier, lifestyle-based preventive measures are left to the individual to enact.
The main economic incentives of preventive health lie with organizations such as payers or employers, who see lower cost or higher productivity with a healthier population.
Payers and employers lack the capability to do long-term, remote monitoring of their covered populations’ health and behaviors, much less tailor incentives to each individual’s unique case.
Preventive measures don’t always lower costs, but most of the time improve outcomes.
Traditionally, payment is based on treatment, not outcomes. Incumbent healthcare industry business models rely on treating sickness (through drugs and devices) instead of preventing it.
To address this challenge, we are interested in scalable technology & business models that enable:
Clear and measurable returns on investment for payers and employers investing in preventive health
Collection, integration, and translation of long-term and/or real-world data for population health stakeholders
Value-based care and other outcome-driven systems
Unaligned system-wide incentives - case in point:
In the US, healthcare and tech giants alike have been making slow (but accelerating) progress on realizing the vision of a value-based care system based on outcomes rather than treatment.
Challenge 3: Lack of actionable information
The field of available health metrics is growing in type, quantity, and complexity. Data needs to be more efficiently collected, processed, and synthesized into evidence-based recommendations in an equitable and inclusive way.
Nearly a quarter of Europeans did not visit a primary care physician in 2017. As a result, an estimated 36% of Europeans living with diabetes are undiagnosed, and a study found 5-10% of UK hospital visitors had undiagnosed (and therefore un-managed) high blood pressure.
We are beginning to understand the implications of “deeper” biomarkers found in genetics, bloodwork, gut microbiome, vital signs, etc. However, this information is not accessible to the average person. For instance, while over half of surveyed Europeans would be interested in knowing their genetic risk profile, only 0.4% of people worldwide have gotten a genetic test. Additionally, most of these studies have been done on populations of European descent, limiting our ability to interpret results from non-white individuals.
Even if information is collected on one’s genetics, blood biomarkers, fitness and diet, these pieces of data often exist on discrete platforms. Aggregating and synthesizing them into evidence-based recommendations is an incredibly complex task.
New medical research emerges daily on behavioral health factors, chronic disease management, and clinical best practices, but is slow to get translated into practice.
To address this challenge, we are interested in scalable technology and business models that unlock:
Cost-effective health and biomarker monitoring
Cost-effective and accessible genetic testing
Translation of complex, multi-dimensional data into precise, effective, actionable insights for behavior change
Data storage, privacy, and security that derisks use of deep personal health data and enables secondary research
Lack of actionable information - case in point:
Chris Hemsworth only discovered his elevated Alzheimer’s risk after getting genetic testing for his most recent movie
Our Investment Thesis:
Opportunities to Build in Preventive Health
As we explore investment opportunities in preventive health, we’ve found it useful to refer to the categorization used in medicine, which breaks preventive care into into four progressive stages, from primary to quaternary. In the table below, we summarize how each stage is defined, and the unique opportunities to make an impact in each.
Opportunity Overview
See footnotes for data sources.1
What’s Being Tried: A Preventive Health Market Taxonomy
To further illustrate the opportunities in each stage of prevention, we created a Preventive Health Market Taxonomy, outlining solution spaces for each stage of prevention and highlighting startups building within them. While by no means exhaustive - we suspect a full market map in this space would contain tens of thousands of startups - we hope this taxonomy gives an idea of what sort of solutions are finding a footing in the market.
In selecting these examples, we considered a few factors:
Geography: Given that healthtech startups must operate under stakeholder dynamics and regulatory environments unique to each country, we aim to offer a comparative approach: these startups represent solutions being attempted across Europe and the United States.
Product-Market Fit: Most startups shown here have raised at least a Series A round, which we take to indicate they have found an approach that has demonstrated some product-market fit.
Relevance to Now: All startups shown are still operational and were founded within the past 10 years.
Explore the interactive version here.
Get in touch!
If these ideas resonate with you, or if you have your own thoughts to add, we’re looking to connect with:
Founders working on innovative and scalable solutions that address one or more of the barriers to preventive health identified above
Like-minded investors who are interested in this space
Companies who are interested in or affected by this space
Experts in preventive health who can help us hone our understanding
Please reach out at sharon@revent.vc.
Opportunity Overview data sources:
The preventable proportion of type 2 diabetes by ethnicity: The Multiethnic Cohort - PMC
New initiative aims to take action on non-communicable diseases | World Economic Forum
Preventive Healthcare Technologies & Services Market Report, 2024
WHO launches global effort to halve medication-related errors in 5 years
Medical Error Reduction and Prevention - StatPearls - NCBI Bookshelf